As we grow older, our bodies undergo natural changes—and our lungs are no exception. For adults over 50, maintaining healthy lungs becomes increasingly important for overall well-being, energy levels, and quality of life. From age-related changes to lifestyle habits, several factors influence lung health in later years. This guide breaks down practical, actionable steps to protect your lungs and recognize early warning signs of trouble.
Understanding Age-Related Lung Changes
First, it’s helpful to know how aging affects the respiratory system. By your 60s, the muscles that help you breathe—like the diaphragm—may weaken, making it harder to take deep breaths. Lung tissue also loses some of its elasticity, reducing the amount of oxygen that enters the bloodstream with each breath. Additionally, the cilia (tiny hair-like structures in the airways that trap dust and germs) become less effective, increasing the risk of infections like pneumonia.
These changes don’t have to lead to breathing problems, though. With proactive care, you can slow down decline and keep your lungs functioning well.
5 Daily Habits to Protect Lung Health
1. Quit Smoking (or Never Start)
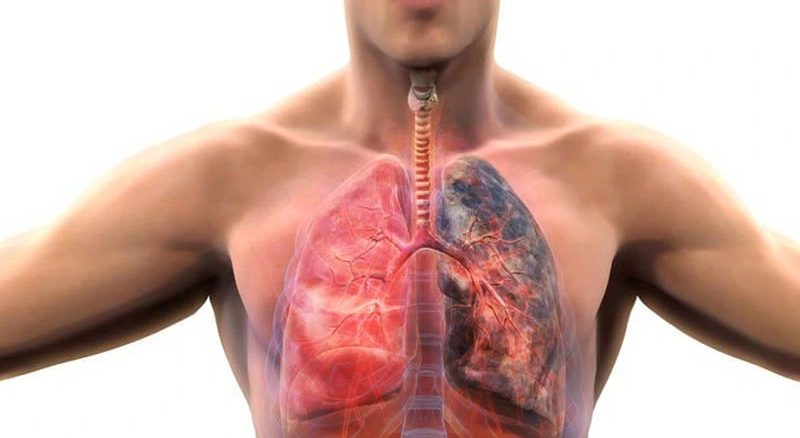
Smoking is the single biggest threat to lung health at any age, but it’s especially harmful for seniors. It accelerates lung tissue damage, increases the risk of chronic obstructive pulmonary disease (COPD)—a leading cause of disability in older adults—and raises the chance of lung cancer.
2. Avoid Pollutants and Irritants
Indoor and outdoor air pollution can irritate sensitive lungs. On days with high air pollution (check local air quality reports), limit time outdoors, especially during morning or evening rush hours when smog is worst.
3. Stay Active with Lung-Friendly Exercise
Regular physical activity strengthens the muscles used for breathing and improves circulation, helping your lungs deliver oxygen more efficiently. You don’t need intense workouts—gentle activities like walking, swimming, or tai chi are ideal for seniors.
4. Get Vaccinated to Prevent Infections
Respiratory infections like the flu and pneumonia can be serious for older adults, often leading to hospitalization or long-term lung damage. Protect yourself by getting annual flu shots and the pneumococcal vaccine.
5. Maintain a Healthy Diet and Stay Hydrated
Eating a balanced diet rich in nutrients supports lung health too. Foods high in antioxidants (like fruits, vegetables, and nuts) help reduce inflammation in the lungs. Staying hydrated keeps mucus thin and easy to clear.
When to See a Doctor: Warning Signs
See your doctor immediately if you experience:
- Persistent cough (lasting more than 3 weeks)
- Shortness of breath during everyday activities
- Chest pain or tightness when breathing
- Wheezing or coughing up blood
- Unintended weight loss or fatigue
Final Thoughts
Taking care of your lungs in your golden years isn’t complicated—it’s about making small, consistent choices that add up. By quitting smoking, avoiding pollutants, staying active, getting vaccinated, and eating well, you can keep your lungs strong and enjoy an active, independent lifestyle.
“It’s never too late to start prioritizing lung health. Talk to your doctor today to create a personalized plan.”