RT’s Three Key Takeaways:
- Critical Gaps in COPD Care – Dr. Haley Hoy’s review highlights major failures in COPD diagnosis and management, including low spirometry use, delayed treatment, and inconsistent adherence to clinical guidelines among primary care providers.
- Barriers on Both Sides – Systemic and patient-level challenges—such as high medication costs, complex inhaler regimens, poor disease understanding, and weak provider-patient communication—continue to hinder effective COPD care.
- Urgency of Early Diagnosis and Education – Hoy emphasizes that early detection, proper maintenance therapy, and patient education are essential to slowing disease progression, reducing exacerbations, and improving long-term outcomes for COPD patients.
COPD impacts hundreds of millions worldwide, yet despite this global toll and the availability of well-established diagnostic tools, countless patients still go undiagnosed in the early stages of the condition, leading to much less favorable outcomes. In a newly published review in Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation, Dr. Haley Hoy of The University of Alabama in Huntsville (UAH) shines a spotlight on gaps in care for this condition, the fourth leading cause of death worldwide.
Hoy, a Certified Registered Nurse Practitioner (CRNP) professor in the College of Nursing at UAH, a part of The University of Alabama System, says the key to meeting the challenges of managing COPD must be addressed from both patient and practitioner perspectives.
“I have always felt a connection with patients diagnosed with COPD,” Hoy says. “COPD is not a reversible condition. It is a progressive disease, meaning lung damage worsens over time, and the airflow obstruction is either irreversible or only partially reversible. In the 25 years I have worked with advanced lung disease patients, there was often very little we could do for this cohort of patients. In the last ten years, that has changed with new therapeutic options now available.”
The condition often presents with comorbidities like cardiovascular disease, musculoskeletal disorders, metabolic disorders, osteoporosis, anxiety, depression and lung cancer. Globally, COPD is the fourth leading cause of death and the eighth leading cause of poor health. In 2020, 480 million, or 10.6%, of people over the age of 25 worldwide suffered from the condition, a number projected to reach approximately 600 million by 2050. The economic burden of COPD in the United States alone is expected to reach $1.037 trillion over the next three decades.
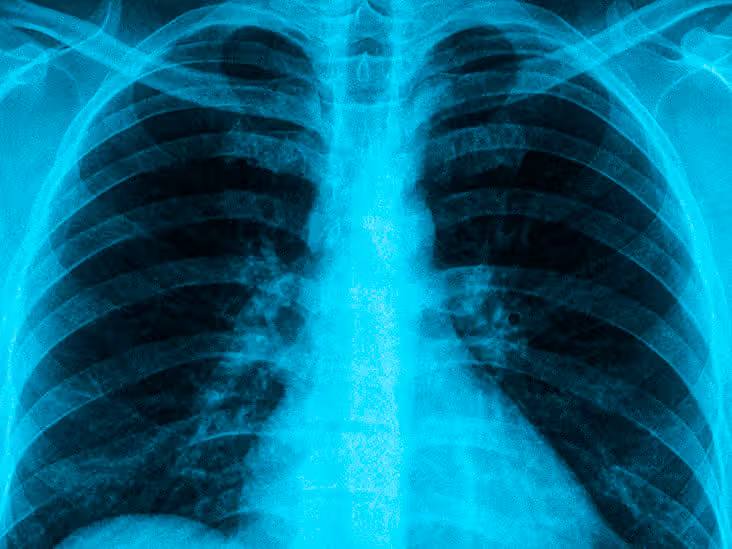
A lung-function test called spirometry, which involves blowing into a machine called a spirometer to record the amount of air a patient can expel, is considered to be the gold standard for diagnosing COPD. The test measures how much and how fast a patient can exhale, crucial for diagnosing the condition, determining its severity, monitoring disease progression, assessing the effectiveness of treatments like bronchodilators, and predicting future risks of complications.
Despite the efficacy of the test, two large US-based studies show the percentage of diagnosed patients who underwent spirometry was low, from 32% to 36.7%, while a European study reveals only 67.6% of patients with physician-diagnosed COPD had undergone spirometry at any point in the past. The inadequate/improper use of spirometry continues to play a major role in the misdiagnosis of COPD.
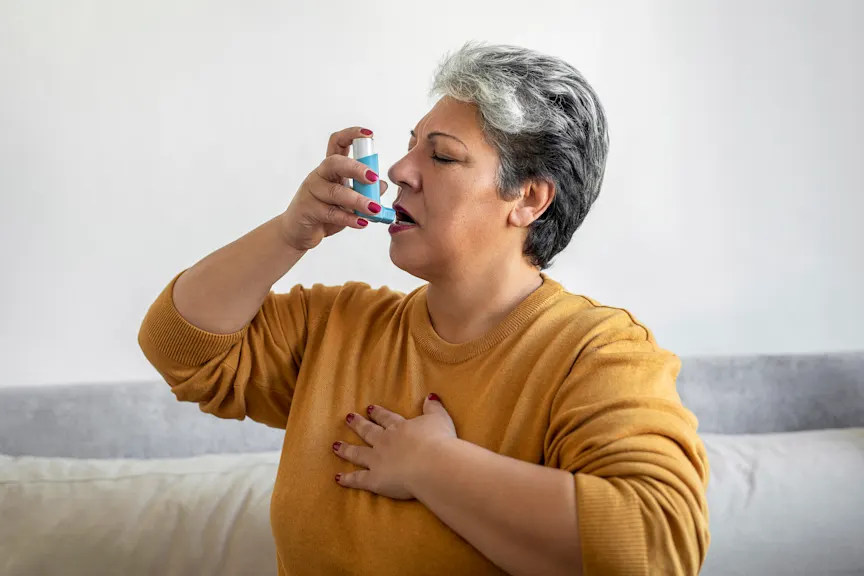
“A major obstacle is the lack of adherence to guidelines by primary care providers, who often manage COPD patients,” Hoy says. “Some of this is due to time constraints during consultations, preventing thorough education on the condition and treatment plan. There is significant confusion related to the number of inhalers available, as well. Also, high costs and complex insurance rules can discourage patients from filling or refilling prescriptions. Some may start with free samples, but stop when they discover their insurance won’t cover the full cost.”
Appropriately administered maintenance pharmacotherapy can significantly reduce symptoms and prevent exacerbations in patients with COPD. However, recent real-world evidence has shown that most patients are not prescribed maintenance pharmacological therapy at initial diagnosis, which can lead to worsening symptoms and increased exacerbations.
Barriers related to the healthcare system include delays in diagnosing COPD and initiating or intensifying treatment, limited provider awareness about treatment guidelines, lack of a positive doctor-patient relationship and an integrated disease management infrastructure, insurance coverage issues and under-diagnosis.
“Patient understanding is paramount in the treatment of COPD,” Hoy says. “Patients may not fully understand their disease, its chronic nature, or the purpose of maintenance therapy, which doesn’t provide immediate relief like a rescue inhaler. A significant communication gap exists, with many patients underestimating the severity of their symptoms.”
Patient-related barriers to care include low socioeconomic status, inadequate family and social support and reluctance to participate in demanding interventions required to manage COPD.
“Complex, multi-dose regimens for inhalers can lead to non-adherence, as can simply forgetting to take medication,” Hoy notes. “Some patients might intentionally skip medication when feeling well due to cost and overuse it during a flare-up. This inconsistent behavior can also lead to under-treatment.”
The ability of individuals who may be susceptible to COPD to recognize symptoms during the early stages of the disease is one of the key criteria for successful early diagnosis and maintenance.
“A delayed diagnosis for a symptomatic COPD patient leads to significantly poorer outcomes, although it does not mean all potential health benefits are lost completely,” the researcher says. “Late-diagnosed patients have a higher rate of exacerbations (flare-ups) and shorter times between episodes. Each exacerbation can cause additional lung damage. Later diagnosis is also linked to higher healthcare resource utilization, poorer quality of life and less time for proactive interventions, such as smoking cessation support and patient education, that can help slow the disease’s progression.”